Keratoconus Causes, Symptoms And 10 Treatment Options
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. This cone shape deflects light as it enters the eye on its way to the light-sensitive retina, causing distorted vision.
Keratoconus can occur in one or both eyes and often begins during a person's teens or early 20s.
Keratoconus Symptoms And Signs
As the cornea becomes more irregular in shape, it causes progressive nearsightedness and irregular astigmatism to develop, creating additional problems with distorted and blurred vision. Glare and light sensitivity also may occur.
Often, keratoconic patients experience changes in their eyeglass prescription every time they visit their eye care practitioner.
What Causes Keratoconus?
New research suggests the weakening of the corneal tissue that leads to keratoconus may be due to an imbalance of enzymes within the cornea. This imbalance makes the cornea more susceptible to oxidative damage from compounds called free radicals, causing it to weaken and bulge forward.
Risk factors for oxidative damage and weakening of the cornea include a genetic predisposition, explaining why keratoconus often affects more than one member of the same family.
Keratoconus also is associated with overexposure to ultraviolet rays from the sun, excessive eye rubbing, a history of poorly fitted contact lenses and chronic eye irritation.
Keratoconus Treatment
In the mildest form of keratoconus, eyeglasses or soft contact lenses may help. But as the disease progresses and the cornea thins and becomes increasingly more irregular in shape, glasses and regular soft contact lens designs no longer provide adequate vision correction.
Treatments for progressive keratoconus include:
- Corneal cross-linking (CXL)
- Custom soft contact lenses
- Gas permeable contact lenses
- Intacs
- Topography-guided conductive keratoplasty
- Corneal transplant
Corneal crosslinking. This procedure, also called corneal collagen cross-linking or CXL, strengthens corneal tissue to halt bulging of the eye's surface in keratoconus.
There are two versions of corneal crosslinking: epithelium-off and epithelium-on.
With epithelium-off crosslinking, the outer layer of the cornea (called the epithelium) is removed to allow entry of riboflavin, a type of B vitamin, into the cornea, which then is activated with UV light.
With the epithelium-on method (also called transepithelial crosslinking), the corneal epithelium is left intact during the treatment. The epithelium-on method requires more time for the riboflavin to penetrate into the cornea, but potential advantages include less risk of infection, less discomfort and faster visual recovery, according to supporters of this technique.
Custom soft contact lenses. Recently, contact lens manufacturers have introduced custom soft contact lenses specially designed to correct mild-to-moderate keratoconus. These lenses are made-to-order based on detailed measurements of the person's keratoconic eye(s) and may be more comfortable than gas permeable lenses (GPs) or hybrid contact lenses for some wearers.
Gas permeable contact lenses. If eyeglasses or soft contact lenses cannot control keratoconus, then gas permeable contact lenses usually are the preferred treatment. GP lenses vault over the cornea, replacing its irregular shape with a smooth, uniform refracting surface to improve vision.
Intacs. These surgically applied corneal inserts manufactured by Addition Technology received FDAapproval for treating keratoconus in August 2004. The tiny plastic inserts are placed just under the eye's surface in the periphery of the cornea and help reshape the cornea for clearer vision.
Intacs may be needed when keratoconus patients no longer can obtain functional vision with contact lenses or eyeglasses.
Several studies show that Intacs can improve the best spectacle-corrected visual acuity (BSCVA) of a keratoconic eye by an average of two lines on a standard eye chart. The implants also have the advantage of being removable and exchangeable. The surgical procedure takes only about 10 minutes.
Intacs might delay but can't prevent a corneal transplant if keratoconus continues to progress.
Topography-guided conductive keratoplasty. While more study is needed, early results of a small study involving topography-guided conductive keratoplasty (CK) show this procedure might help smooth irregularities in the corneal surface.
Corneal transplant. Some people with keratoconus can't tolerate a rigid contact lens, or they reach the point where contact lenses or other therapies no longer provide acceptable vision. The last remedy to be considered may be a cornea transplant, also called a penetrating keratoplasty (PK or PKP). Even after a transplant, you most likely will need glasses or contact lenses for clear vision.
Electrophysiology testing includes a battery of tests which can be used to provide information about the visual system beyond the standard clinical examination of the eye. Electroretinography (ERG) and Electro-oculography (EOG) are two of the tests conducted in the Ophthalmic Electrophysiology Laboratory. The primary objective of the electrophysiologic examination is to assess the function of the visual pathway from the photoreceptors of the retina to the visual cortex of the brain. Information obtained from these diagnostic tests helps establish the correct diagnosis or may rule out related ophthalmic diseases.
Electrophysiologic testing is useful in diagnosing a variety of inherited retinal and optic nerve diseases, toxic drug exposure, inflammatory conditions, intraocular foreign bodies, and retinal vascular occlusions. Electrophysiologic testing is performed most often in large referral centers which have expertise in obtaining and interpreting these data. The data are used in conjunction with the clinical examination and other tests (perimetry, dark adaptometry) to establish a correct diagnosis.
The Electrophysiology Service at the University of Iowa specializes in:
- Standardized full-field electroretinography (ERG)
- Multifocal electroretinography (mfERG or mERG)
- Dark adaptometry
Electrodes Used:
- Burian-Allen Electrode
- DTL Plus Electrode
Full Field Electroretinography (ERG)
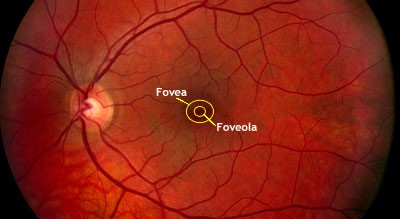
Full Field Electroretinography (ERG) is a test used to detect abnormal function in the retina (the light-detecting portion of the eye). Specifically, this test examines the function of the light-sensitive cells of the eye (the photoreceptors), and several other cells that process these light signals before they are sent to the brain. Photoreceptors are specialized nerve cells in the eye that are sensitive to light. There are two types of photoreceptors in the human eye: rods and cones. Cones provide central high-acuity vision used for reading and are also color vision. There are 6 to 7 million cones in the retina, of which about 650,000 are concentrated in the foveola for central vision. Rods provide vision in dim light. There are about 120 million rods in the retina, of which none are located in the foveola.
During the ERG test, the photoreceptors produce tiny amounts of electricity in response to brief flashes of light. If we know exactly how much light enters the eye, and how much electrical response is generated, we can figure out how well the rods and cones are working. The differences in responses are analyzed to differentiate diseases which affect the rods from those which affect the cones or other cells
To detect the electrical response of both the rods and the cones, special electrodes are placed on the surface of the eye. There are several types of electrodes; the type of electrode used will depend on the type of test being performed, the age of the patient, and the suspected condition.
How is an ERG done?
The patient assumes a comfortable position (lying down or sitting up). Usually the patient's eyes are dilated beforehand with standard dilating eye drops.
The patient will be asked to sit in the dark for 20 minutes. The patient may have someone sit with them or they may listen to music, but they will not be able to use any device that will emit a light. This allows the eyes to adjust to the darkness so that the function of the rod photoreceptors can be examined. After sitting in the dark, the technician will place numbing drops in the eyes. The patient is asked to look up, and an electrode is gently placed on each eye. Some electrodes are contact lenses with small wires attached; others are fine threads that lay across the surface of the eye. An additional electrode is placed on the forehead.
The test is painless. However, the electrode that rests on the eye may feel a little like an eyelash is in the eye. This sensation may persist up to several hours following completion of the ERG. One should not rub the eyes for at least an hour after an ERG (or any test in which the cornea has been numbed), to avoid scratching the cornea.
Flashes of light are used to stimulate the retina. The first light is so dim that only the rods respond. The response is sensed by the electrode, amplified, and displayed on a computer screen. The intensity of the testing light is progressively increased. We refer to this as the dark adapted phase and this part of the test may take 10 to 15 minutes.
Flashes of light are used to stimulate the retina. The first light is so dim that only the rods respond. The response is sensed by the electrode, amplified, and displayed on a computer screen. The intensity of the testing light is progressively increased. We refer to this as the dark adapted phase and this part of the test may take 10 to 15 minutes.
How to prepare for the test
No special preparation is necessary for this test. We ask that you do not wear any eye make-up the day of testing.
What is a normal outcome for an ERG?
A normal ERG contains an a-wave (initial negative deflection) followed by a b-wave (positive deflection). The leading edge of the a-wave is produced by the photoreceptors, while the remainder of the wave is produced by a mixture of cells.
What does an abnormal ERG mean?
An abnormal ERG result suggests abnormal function of the retina which may be caused by a number of diseases of the retina. The results of the ERG will be discussed with your doctor.
ERG under anesthesia
An electroretinogram (ERG) can be performed in the operating room under general anesthesia in children who are too young to understand and perform the test in the clinic. Children will first be evaluated in the clinic by Dr. Arlene Drack. If it is determined that an ERG under anesthesia is necessary, a pre-operative elevation will be conducted which will determine the need for a further anesthesia work up. The ERG performed in the operating room is very similar to the ERG preformed in the clinic. The dark adaptation is done under anesthesia, and then both the dark adapted and light adapted responses are recorded. The ERG under anesthesia takes approximately 90 minutes to perform.
Multifocal Electroretinography (mfERG)
Multifocal techniques, in particular the multifocal ERG, are used in the diagnosis of ophthalmological diseases. The mfERG is a technique for assessing the local ERG from different regions of the retina. The mfERG is particularly valuable in cases in which the retina appears normal and it is difficult to distinguish between diseases of the retina and diseases of the optic nerve.
Electrical responses from the eye are recorded with an electrode just as in conventional ERG recording, but the special nature of the stimulus and analysis produces a more detailed map of where in the central retina ERG responses are normal or abnormal. This can help distinguish among different diseases.
For the routine mfERG, the retina is stimulated with a pattern of hexagons. The pattern will seem to flicker randomly, but each element follows a fixed, predetermined sequence called an ‘m sequence’. By correlating the continuous ERG signal with the on or off phases of each stimulus element, the focal ERG signal associated with each element is calculated.
How is the mfERG done?
As in full field ERG the patient assumes a comfortable seated position. Usually the patient's eyes are dilated beforehand with standard dilating eye drops. The technician will place a numbing drop in the eye. The patient is asked to look up, and an electrode is gently placed on the eye. An additional electrode is placed on the forehead. The eye not being tested is covered with a black eye patch.
The patient will be asked to continuously look at an ‘X’ located in the center of a monitor. The monitor will display a flashing hexagon pattern for 30 seconds, and then stop. This will be repeated 8 times for each eye. The test will take approximately one hour to complete.
How to prepare for the test
No special preparation is necessary for this test. We ask that you do not wear any eye make-up the day of testing.
What is the outcome for a mfERG?
Data can be displayed in various ways, such as waveform traces or colored graphs. The results of the mfERG will be given to your doctor for analysis and may be discussed with you at a later date.
Dark Adaptometry (DA)
Dark adaptometry (DA) measures the eye’s ability to detect a dim light, a measure of rod photoreceptor function. Two values are measured: the dimmest light the eye can detect the dark adaptation threshold and the time it takes to detect a dim light after going from condition of bright light to darkness, dark adaptation curve. Dark adaptometry may be used in concert with other tests such and the ERG or mfERG.
How is the test done?
Dark Adaptation Curve
The test is performed in a dark room. The patient will hold a special light to their eye and look at a bright light for 1 minute. After 1 minute, the patient will be asked if they can see another dimmer light. The light will continue to be presented at regular intervals until it is seen. Once seen, the light will be dimmed more and the test will continue until the dimmest light is no longer seen. The time at which each light intensity is seen is documented and recorded on a graph. This test will take approximately 30 to 45 minutes to perform.
Dark Adaptation Threshold
This test is performed in a dark room, after the patient is asked to sit in the dark for 30 to 45 minutes. This allows the eyes to be their most sensitive for the light. A light is presented to the patient and its brightness is changed until the dimmest light that can be seen has been determined. This process usually takes 3-5 minutes.
Types of Electrodes
Burian-Allen Electrodes
Burian-Allen Electrodes are bipolar, reusable contact lens electrode with built-in lid speculum and lead wire. They are available in a number of sizes. We use these electrodes mainly on sedated patients.
DTL Plus Electrodes
DTL Plus Electrodes are disposable, mono-polar Silver-Nylon thread electrode with adhesive fasteners. This is our main electrode.
What Are Implantable Contact Lenses?
Wanting to see clearly is more than just a convenience. If you are one of the nearly 8 million Americans with visual difficulties, wearing glasses or contact lenses is an absolute necessity that is sometimes not enough. Implantable contact lenses (ICL) are one answer that may eliminate the need for glasses.
Visian ICL vs LASIK Eye Surgery
While not everyone has heard of Visian ICL for vision correction, many people have heard of LASIK eye surgery. These two procedures are both used to correct mild to moderate vision problems, but they are very different approaches to vision correction.
The LASIK eye procedure changes the shape of the cornea to adjust myopia (nearsightedness) or hyperopia (farsightedness). This allows the cornea to focus light better on the retina, resulting in clearer images.
By comparison, Visian ICL is inserting a contact lens implant into the eye to correct mild to severe myopia. Implantable contact lenses are replaceable should your vision results change, and they do not affect the shape or function of the cornea. The lenses are not felt by the wearer, and cannot be seen by others.
Who is a Candidate for Visian ICL?
If you want surgical vision correction, you must be in good general health and be able to go through the short surgery and a mild recovery period. Visian ICL is not designed to correct age-related vision problems such as presbyopia, so ideal candidates for the procedure are adults under age 45. However, if you initially thought about having LASIK eye surgery and were not listed as a good candidate you may still be able to have the Visian ICL procedure.
Reasons for not being thought an appropriate candidate for LASIK include the:
- Severity of your myopia
- Presence of chronic dry eye symptoms
- Shape or thickness of your cornea
What are Implantable Contact Lenses?
If you can imagine a contact lens on the outside of your eye, you have a good sense for the way contact lens implants work. The American Academy of Ophthalmology notes that they are much like contact lenses, in that they focus light onto your retina in a way that makes the images you see much sharper.
These implantable lenses are called phakic intra-ocular lenses, meaning lenses for people who still have their natural eye lenses. Your doctor will make a prescription for the lenses that should correct your myopia. At this time, Visian ICL can only address myopia, however, STAAR Surgical Company has established studies in Europe that may eventually lead to the release of toric ICL lenses in the United States; these correct for astigmatism as well as myopia.
How is Visian ICL Done?
During your ICL procedure, the implantable contact lens will be inserted between the iris and natural lens of your eye. When it is time to implant the lenses, the surgeon places a gel into the eye to protect against any damage during the surgery. The surgeon makes very small incisions in the cornea to allow the placement of a tiny cartridge that holds the ICL. After the lens unfolds completely, the surgeon tucks the corners of the lens behind the iris, so that the lens becomes completely invisible. The surgeon then makes one small incision in the iris (the colored part of the eye) to allow fluid to circulate around the lens. The process for each eye takes about 10 to 15 minutes.
What if My Lens Prescription Changes?
There are two notable benefits to Visian ICL, 1) that they are effective and 2) that they can be replaced as vision prescriptions change. Should you need to change your lenses or add reading glasses to manage your developing age-related vision changes, contact lens implants will offer you that flexibility. When the time comes if Visian ICL sounds good to you, the surgeon can give you more information about what to do to ensure the best result from implantable contact lenses.
How Much Does Visian ICL Cost?
Like LASIK eye surgery, Visian ICL is usually not covered by your insurance. However, this does not mean that the surgery is out of your reach. When you look at it as a long-term investment in your health and ability to see properly, it is easier to consider the expense.
If you were disappointed to learn that you could not have LASIK eye surgery, Visian ICL may be an option to correct your myopia.